Dental Implant Health: A review of definitions & recommendations for care
Peri-implant mucositis: A reversible inflammatory reaction in the soft tissues surrounding a
functioning implant. Treating this condition will prevent peri-implantitis! Similar to gingivitis around a natural tooth.
Peri-implantitis: A destructive inflammatory reaction affecting the soft (gingiva) and hard (bone). Similar to periodontal disease with loss of attachment in a natural tooth.
functioning implant. Treating this condition will prevent peri-implantitis! Similar to gingivitis around a natural tooth.
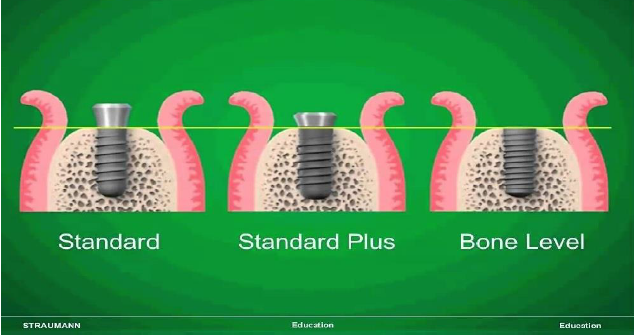
Different implant systems have different methods of placement.
Tissue level implant (Pictured below, 2 images to the left): The implant has a rough surface, which is placed down to the bone crest, and a polished collar (all one part of implant) extends to the gingival margin. Bone levels should maintain at the top of the rough surface.
Bone level implant (Pictured below, right image): The implant has a fully roughened surface and is placed equal to the bone crest. A separate restorative abutment is later connected that extends up to the gingival margin. Bone levels should maintain at the top of the rough surface.
Clinical assessments (visual, probing and radiographs) that will be performed by your dental professional to determine the health of your dental implant.
Visual: Evaluate for plaque, tartar or cement, gingival tissue color, texture and keratinized (attached) vs. non-keratinized tissue (unattached).
Clinical assessment: Your dental professional will be able to identify different implant systems and whether it is a tissue level or bone level implant, check for movement, and check the bite. As with natural teeth, implant mobility should be assessed using the flat ends of hand instruments. True mobility of an implant is a lack of osseointegration (attachment to the bone) that will require removal of the implant. However, clinical evaluation should include a check for other prosthetic issues, such as a loose implant crown, abutment or screw. If the implant body is mobile, it’s a failure.
Probing: The tissues around dental implants have a weaker attachment, bleed easier, and are more sensitive to probing. Use light pressure and a plastic probe. Profuse bleeding, suppuration, and increasing pocket depth require attention/action.
Radiographs (x-rays) will be taken to compare to baseline x-rays to evaluate for bone loss.
Periodontal maintenance procedure (dental hygiene visits and cleanings are often performed 3 or 4 times a year for patients with dental implants)
Evaluation and documentation
Removal of all soft and hard deposits, often using specialized dental implant plastic or titanium instruments. If infection is present, use whatever necessary to debride and decontaminate the implants. A person's bite should be checked regularly.
Reinforcing daily biofilm (plaque) removal with at home oral hygiene instructions and customized daily oral hygiene strategies. I do agree with using Listerine (diluted with water if strong alcohol content is an issue), power toothbrush, Proxysoft Bridge and Implant Floss (www.proxysoft.com), double-bend end tufted brush for lingual of lower hybrids (Tepe brand) Waterpik only if the patient has proven non-complaint to all other suggestions after multiple times (with instruction to keep on a low setting and 90 degree angle).
Determination of hygiene maintenance schedule – Every 3 to 4 months if less than ideal periodontal health, advancing age, or systemic health conditions.
Care for Peri-implant mucositis or Peri-Implantitis
Suspected Peri- Implant Mucositis: Your dental professional can attempt to treat this condition with non-surgical therapy and daily disease control (effective oral hygiene). Reevaluate and reassess. If the issue cannot be resolved in six months, refer to your implant specialist.
Suspected Periimplantitis: Non-surgical therapy is typically ineffective unless an obvious piece of cement or debris can be removed. This is because of the complex structure of the implant prosthesis, rough surface or implant threads. Your dentist will then refer you to an implant specialist to see if a restorative issue can be addressed, or if surgical (traditional or laser LAPIP therapy https://www.lanap.com/lanap/what-is-lapip), or implant removal is needed.

Britten Periodontics & Implant Dentistry is a periodontal practice offering patients personalized dental care in implant dentistry in Clearwater, Florida. Dr. Todd Britten received his Bachelor of Science & Doctorate of Dental Surgery from University of Florida, a Master’s Degree and Certificate in Periodontology and Implant Dentistry; and completed extensive training at the Institute of Advanced Laser Dentistry. He is one of the only board-certified periodontists in Pinellas County. He is a member of the American Academy of Periodontology, American Dental Association, Florida Association of Periodontists, Upper Pinellas County Dental Association, Hillsborough County Dental Association, Hillsborough County Dental Research Association and Florida West Coast Dental Association.
To learn more about Dr. Britten and his dental services, call (727) 586-2681 or visit our website at www.brittenperio.com